Introduction:
Venus leg ulcers, diabetic leg ulcers, and chronic wounds present significant challenges in healthcare due to their complex etiology and prolonged healing times. In this article, we explore comprehensive management strategies tailored to address the unique characteristics of these conditions, aiming to promote healing and improve patient outcomes.
Understanding Etiology and Risk Factors:
Effective management begins with a thorough understanding of the underlying etiology and risk factors contributing to venous leg ulcers, diabetic leg ulcers, and chronic wounds. Venous leg ulcers often result from venous insufficiency, while diabetic leg ulcers stem from neuropathy, peripheral vascular disease, and impaired immune response. Chronic wounds can arise from various factors, including pressure, trauma, infection, and systemic diseases.
Assessment and Diagnosis:
Accurate assessment and diagnosis are essential for guiding appropriate treatment interventions. This involves evaluating the size, depth, location, and characteristics of the chronic wound, as well as identifying any underlying vascular or neuropathic complications. Imaging studies, such as Doppler ultrasound and MRI, may be utilized to assess vascular perfusion and tissue viability.
Wound Debridement:
Debridement, the removal of necrotic tissue and foreign debris, is a fundamental aspect of wound management. It promotes wound bed preparation, enhances the effectiveness of subsequent therapies, and reduces the risk of infection. Debridement methods may include sharp debridement, enzymatic debridement, autolytic debridement, and surgical debridement, selected based on the wound’s characteristics and patient’s tolerance.
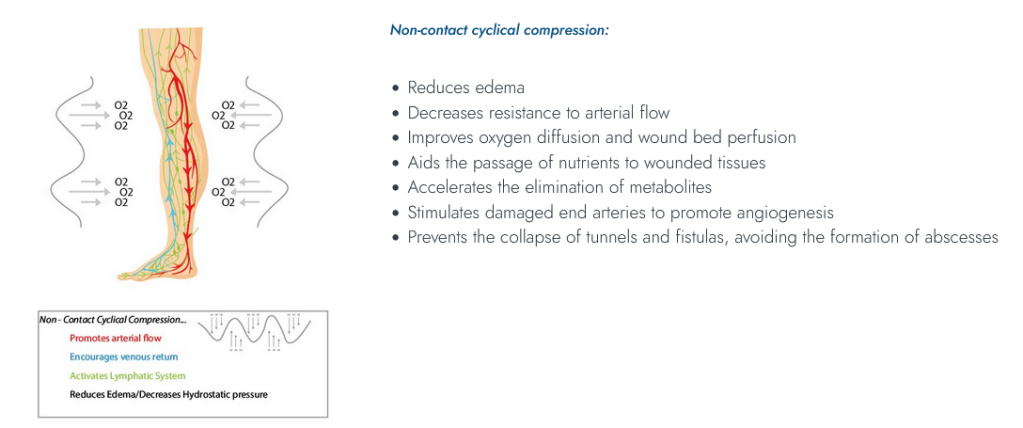
Compression Therapy for Venus Leg Ulcers:
Compression therapy plays a central role in managing venous leg ulcers by improving venous return, reducing edema, and promoting tissue healing. Graduated compression bandaging or compression stockings are commonly used modalities to apply consistent pressure to the affected limb. Careful assessment of arterial perfusion is necessary before initiating compression therapy to prevent ischemic complications.
Offloading and Pressure Redistribution for Diabetic Leg Ulcers:
Offloading the affected foot is critical in diabetic leg ulcer management to relieve pressure on the wound site and prevent further tissue damage. Total contact casts, custom orthotics, and specialized footwear can help redistribute pressure and provide protection to at-risk areas. Regular monitoring of foot sensation and vascular status is essential to identify early signs of neuropathy or peripheral arterial disease.
Advanced Wound Dressings and Topical Therapies:
The selection of appropriate wound dressings and topical therapies is guided by the wound’s characteristics, such as moisture level, exudate amount, and presence of infection. Advanced dressings, including hydrogels, hydrocolloids, foams, and alginate dressings, promote a moist wound environment, facilitate autolytic debridement, and enhance granulation tissue formation. Topical agents such as antimicrobials, growth factors, and bioengineered skin substitutes may be utilized to stimulate wound healing and control infection.
Multidisciplinary Collaboration and Patient Education:
Successful management of venous leg ulcers, diabetic leg ulcers, and chronic wounds requires a multidisciplinary approach involving collaboration between wound care specialists, vascular surgeons, podiatrists, diabetes educators, and other healthcare professionals. Patient education regarding wound care, self-management strategies, lifestyle modifications, and preventive measures is essential to empower individuals to actively participate in their healing process and reduce the risk of recurrence.
Conclusion:
Effective management of venous leg ulcers, diabetic leg ulcers, and chronic wounds necessitates a comprehensive and individualized approach that addresses the underlying etiology, promotes wound healing, and prevents complications. By integrating strategies such as assessment, debridement, compression therapy, offloading, advanced dressings, topical therapies, multidisciplinary collaboration, and patient education, healthcare providers can optimize outcomes and improve the quality of life for individuals living with these challenging conditions.